Inflammatory bowel syndrome...what is it?Anyone that's diagnosed with it, would say it's frustrating, because it isn't really a diagnosis. Inflammatory bowel syndrome, or IBS, is the diagnosis you're given when everything else has been ruled out. It's a collection of symptoms with an origin that can't be identified. 40% of people that visit the doctor report gastrointestinal problems. 60 million Americans suffer from IBS and those are only those that have received the "diagnosis."  Symptoms may include:
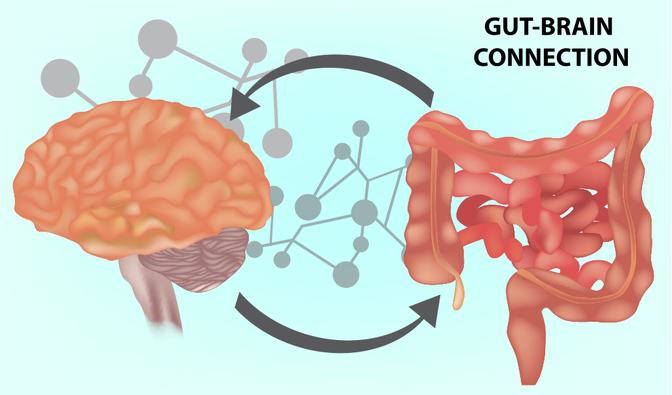
Symptoms may also include headaches, fatigue, insomnia, and/or muscle pain. To receive a diagnosis of IBS, the symptoms are chronic, occurring for at least three to six months. What causes IBS?Previously, it was thought that IBS was a psychosomatic issue, that it was caused by real or perceived stress. In other words, that is was all in the head. Wouldn't it be nice if you could control your symptoms by adjusting your mindset. IBS is now classified as a gut-brain axis problem. However the more that's learned about the gut-brain axis, the more researchers realize that the communication pathway between the gut and brain is bidirectional and IBS is much more than a psychological condition. IBS is caused by any combination of factors that can disrupt the nervous system in the gut, the production of digestive enzymes, and the muscular reflex system. The root causes of IBS can be Small Intestinal Bacterial Overgrowth (SIBO), food intolerances, leaky gut, parasites living in the gut, yeast overgrowth, zinc or magnesium deficiency, or heavy metal toxicity. Because there's commonly a disruption of the nervous system and reflexes is why IBS is categorized as a gut-brain axis dysfunction. What's the gut-brain axis?The gut-brain axis is a bidirectional communication between the brain and the gut. We all know that the brain is a big control area for our nervous system. What many of us don't know is that the gut also has a nervous system, called the enteric nervous system. The enteric nervous system is part of the autonomic nervous system. It controls all muscle contractions and reflexes that happen during digestion. IBS is characterized by a disturbance in the autonomic nervous system. What used to be described as a motility dysfunction, is now being looked at as a breakdown in communication between the gut and brain. The result is that the body starts responding to stimuli that normally wouldn't be painful, also known as hypersensitivity. The interesting part is that it was thought that it was the brain that was in charge of the digestive system, but researchers are observing that the gut is in control as well. The gut is more recently considered to be the second brain, in fact it has more neurons than the brain and spinal cord put together. Neurons communicate and transmit information throughout the body using neurotransmitters. The brain sends many important signals using neurotransmitters and as the biggest sensory organ, the gut also sends important signals. The gut has the same variety of twenty to thirty different neurotransmitters that the brain has, which means that the gut has the same capability to communicate as the brain. Not only that, but the relative small number of nerve fibers that connect the brain to the gut (only 1200), is what leads researchers to believe that the gut really has a mind of it's own. How complex is the gut?The digestive processes are critical and complex. Neurons in the gut control the mechanical and chemical processes involved in digestion, which means they control the reflexes and also signal the release of the necessary enzymes and hormones.  It seems there's more going on in the gut than just digestion. Chances are you've probably had that feeling of butterflies in your stomach when you're nervous or excited about something. Or that feeling of dread in the pit of your stomach. It turns out that 90% of serotonin, the happiness neurotransmitter, is produced and stored in the gut. There are tons of serotonin receptors in the gut. Serotonin is also in control of motility, or movement of the contents of the gut. So when serotonin uptake is inhibited, the serotonin receptors become desensitized over time, which can result in constipation. An imbalance can also cause too much stimulation which can result in diarrhea. It's not clear exactly how serotonin in the gut affects the brain, but many neurological conditions are linked to IBS symptoms and vice versa. Serotonin also plays a role in sleep, mood, appetite, and pain sensitivity, as well as transporting regulatory messages, so it can alter the volume of a signal or the degree of a particular response. The gut also produces four other important neurotransmitters that are found in both the brain and the gut: GABA, Brain-derived neurotrophic factor, or BDNF, norepinephrine, and dopamine. Bacteria in our gut create many of these neurotransmitters, which supports the idea of there being a brain in the gut. It's been my experience with myself and with my son, that there is a correlation between conditions in the gut and conditions in the brain and numerous studies support this. About 66% of people with IBS, also fit the criteria for a mood disorder. Antidepressants are one of the most common treatments prescribed for IBS. The neurotransmitters in the gut may explain why serotonin and norepinephrine inhibitors have been found to be effective medications for this. Is the inflammation just in the gut?I've written quite a lot about chronic inflammation and it does seem that inflammation in the gut can spread throughout the entire body, including the brain. This can affect neurodevelopment, the brain's development at birth, and also neurodegeneration, the aging of the brain. Many kids with autism also have gastrointestinal issues, thus many researchers are working on better understanding the second brain to find clues on just how they're connected. Getting to the root causes and solutionsThere isn't one solution for everyone with IBS. It's a complex problem with many different causes that can overlap, just like stress doesn't come from just one part of your life. Since there are both physiological psychosocial components of IBS, it follows that you need to work on both. Mental stress may contribute to IBS and so stress reduction techniques like those I wrote about last week will definitely help. However, they need to go hand in hand with dietary changes to heal the gut, like I wrote about here. The most commonly recommended diets for those diagnosed with IBS are the Low-FODMAP diet and the GAPS diet. Both of them are more restrictive than a general healthy lifestyle diet. It's generally recommended to try these diets relatively short term, or until the symptoms of IBS are well under control, then you can continue with what I call a general healthy lifestyle diet. FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. They are different types of sugars and starches, or short-chain carbohydrates. Often people with IBS have trouble digesting short-chain carbohydrates. Foods are divided into low-FODMAP foods, which are okay to eat, and high-FODMAP foods, which are to be avoided. The low-FODMAP diet can be tried for six weeks, then foods can be introduced one at a time, keeping note of any trigger foods. For more information on how to follow an elimination diet, click here, and be sure to download the guide that goes along with it. If following the low-FODMAP or GAPS diet seems overwhelming, try cutting foods out one or a few at a time. Generally, cutting out caffeine is a good first step if you're suffering from IBS, followed by drinks that contain fructose or artificial sweeteners. Next, alcohol, lactose, legumes, and any other foods that might be irritating to the digestive system should be eliminated. Just remember, these changes and diets aren't meant to be permanent. Follow them as long as it takes to heal, then introduce specific foods back in moderation. Do you have personal experience with IBS? Have you noticed a correlation between IBS and other symptoms, such as mood?
1 Comment
Jean Mumford
7/26/2018 05:32:54 pm
I had IBS for years. I stopped drinking coffee and it went away. Have not had a problem since.
Reply
Leave a Reply. |
Click below to join my FREE Facebook Group-
Women's Wellness Circle: Create Your Extraordinary Life AuthorHi, I’m Crystal! If you'd like to access my Farmer's Market Friday posts from 2018, click here!
Categories
All
|

 RSS Feed
RSS Feed